ERN ReCONNET
Disease Info
Disease: Antiphospholipid Syndrome
Antiphospholipid Syndrome (APS)
Overview – What is APS?
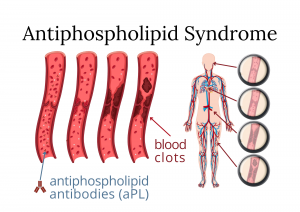
Antiphospholipid syndrome (APS) is a systemic autoimmune disease characterized by arterial, venous, or small vessel thromboembolic events and/or obstetric morbidity in the presence of persistent circulating antiphospholipid (aPL) antibodies detected by means of three tests: lupus anticoagulant, anticardiolipin, and beta-2 glycoprotein I antibodies.
APS can occur as an isolated condition, known as, “Primary APS”, or it can occur in the setting of another systemic autoimmune disease, particularly with systemic lupus erythematosus (SLE).
Epidemiology
The actual incidence of APS is unknown. APS is more common in women than in men. Having another autoimmune condition, such as SLE, increases the risk of APS. Estimates have indicated an incidence of around 5 new cases per 100,000 persons per year, with a prevalence of around 40-50 cases per 100,000 persons. aPL are positive in approximately 13.5% of patients with stroke, 11% with myocardial infarction, 9.5% of patients with deep vein thrombosis, and 6% of women with pregnancy morbidity.
References:
– Petri M. Epidemiology of Antiphospholipid Syndrome. In: Hughes Syndrome. London: Springer-Verlag; 2006.
– Andreoli L, et al. Estimated frequency of antiphospholipid antibodies in patients with pregnancy morbidity, stroke, myocardial infarction, and deep vein thrombosis: a critical review of the literature. Arthritis Care Res (Hoboken) 2013.
– Radin M, et al. Antiphospholipid Syndrome is still a rare disease: the estimated prevalence in Piedmont and Aosta Valley. Arthritis Rheumatol 2020.
– Duarte-García A, et al. The Epidemiology of Antiphospholipid Syndrome: A Population-Based Study. Arthritis Rheumatol 2019.
Causes
The cause of APS is not entirely understood. Like other autoimmune diseases it is thought to be multifactorial and that genetic, hormonal and environmental factors play a significant role in developing the disease. APS occurs when the immune system mistakenly produces antibodies that make blood much more likely to clot.
APS can occur as an isolated condition, known as, “Primary APS”, or it can occur in the setting of another systemic autoimmune disease, particularly with systemic lupus erythematosus (SLE).
The actual incidence of APS is unknown. APS is more common in women than in men. Having another autoimmune condition, such as SLE, increases the risk of APS. Estimates have indicated an incidence of around 5 new cases per 100,000 persons per year, with a prevalence of around 40-50 cases per 100,000 persons. aPL are positive in approximately 13.5% of patients with stroke, 11% with myocardial infarction, 9.5% of patients with deep vein thrombosis, and 6% of women with pregnancy morbidity.
– Petri M. Epidemiology of Antiphospholipid Syndrome. In: Hughes Syndrome. London: Springer-Verlag; 2006.
– Andreoli L, et al. Estimated frequency of antiphospholipid antibodies in patients with pregnancy morbidity, stroke, myocardial infarction, and deep vein thrombosis: a critical review of the literature. Arthritis Care Res (Hoboken) 2013.
– Radin M, et al. Antiphospholipid Syndrome is still a rare disease: the estimated prevalence in Piedmont and Aosta Valley. Arthritis Rheumatol 2020.
– Duarte-García A, et al. The Epidemiology of Antiphospholipid Syndrome: A Population-Based Study. Arthritis Rheumatol 2019.
The cause of APS is not entirely understood. Like other autoimmune diseases it is thought to be multifactorial and that genetic, hormonal and environmental factors play a significant role in developing the disease. APS occurs when the immune system mistakenly produces antibodies that make blood much more likely to clot.
Maria Tektonidou
Maria Tektonidou
Disease Coordinator
Disease Coordinator
Silvia Aguilera
ePAG representative
ePAG representative
Savino Sciascia
Savino Sciascia
Disease Coordinator
Disease Coordinator
Jamy Scheerhoorn-Pullen
ePAG representative
ePAG representative
Common symptoms
Thrombosis (blood clot) – Venous or arterial thrombosis:
- Deep venous thrombosis – Blood clots in legs, leading to local pain, swelling and redness of the skin.
- Transient ischemic attack (TIA) – Similar to a stroke, but usually lasts only a few minutes and causes no permanent damage.
- Stroke
- Heart attack
In addition to thrombotic events, obstetric complications are the other hallmark of APS. These include:
- Embryonic losses – early recurrent miscarriages (<10 weeks gestation)
- Fetal loss (after 10th week)
- Premature births (<34 weeks) – due to severe preeclampsia or placental insufficiency
Other manifestations include:
- Livedo reticularis – a mottled reticulated vascular pattern that appears as a lace-like purplish discoloration of the skin
- Rash
- Low blood platelet count (thrombocytopenia) – the decrease in platelets can lead to episodes of bleeding.
Rarely, a life-threatening form of multiorgan thrombosis, known as catastrophic APS (CAPS), can occur.
When to see a doctor?
If you develop any of the symptoms above, make an appointment with a doctor, especially if they are severe, persistent, and recurrent. Once you have a diagnosis established, the rheumatologist may schedule regular visits. APS can cause blood clots, which can be fatal. Seek emergency care if you have signs and symptoms of:
- Swelling, pain, or warmth in the arms or legs
- Chest pain
- Shortness of breath
- Racing heart
- Coughing up blood-streaked mucus
- Confusion
- Sudden numbness, weakness or paralysis of your face, arm or leg
- Difficulty speaking or understanding speech
- Visual disturbances
- Severe headache
Diagnostics tests
Screening for antiphospholipid antibodies should be performed if there is a clinical suspicion of APS. Laboratory confirmation of the presence of antiphospholipid antibodies on 2 occasions at least 12 weeks apart is required for the diagnosis. Antiphospholipid antibodies include the following:
- Lupus anticoagulant
- Anticardiolipin antibody
- Anti-beta2-glycoprotein I antibody (anti-B2GP-I antibody)
Other laboratory investigations should include the following:
- Complete blood count
- Serum creatinine, liver function tests
- ANA – antinuclear antibodies, anti–dsDNA antibodies
- C-reactive protein (CRP)
- Erythrocyte sedimentation rate (ESR)
- Urinalysis with microscopic analysis
- Other tests (protein electrophoresis, complement C3 and C4)
Investigations to consider:
- Venous Doppler ultrasound
- Chest X-ray
- CT angiogram of the chest,
- Cranial MRI
- Echocardiography
- Inherited thrombophilia tests
How to Interpret Antiphospholipid Laboratory Tests
aPL antibodies included in the classification criteria can be one of three types: lupus anticoagulant, anticardiolipin antibodies or antibeta2 glycoprotein I antibodies. The most important aPL antibody is the lupus anticoagulant, due to its strong association with both thrombotic and obstetric morbidities.
Generally, the diagnosis is made in the presence of one or more of the above aPL in the setting of a vascular thrombosis or a specific obstetric morbidity. Individuals with positivity for one or more aPL antibodies, but without a history of thrombosis, obstetric morbidity, or other clinical manifestations have a higher risk in developing APS.
Classification criteria
Antiphospholipid syndrome can be diagnosed if at least one of the clinical and one of the laboratory criteria that follow are met:
– Clinical criteria
- Vascular thrombosis
– One or more clinical episodes of arterial, venous (except superficial vein thrombosis), or small vessel thrombosis, in any tissue or organ. Thrombosis must be confirmed by objective diagnostic tests.
- Pregnancy loss
- One or more unexplained deaths of a morphologically normal fetus at or beyond the 10th week of gestation, with normal fetal morphology, or
- One or more premature births of a morphologically normal neonate before the 34th week of gestation because of: eclampsia, severe pre-eclampsia, or recognized features of placental insufficiency, or
- Three or more unexplained consecutive spontaneous abortions before the 10th week of gestation, with maternal anatomic or hormonal abnormalities and paternal and maternal chromosomal causes excluded.
– Laboratory criteria*
- Lupus anticoagulant (LA) present in plasma, on two or more occasions at least 12 weeks apart.
- Anticardiolipin (aCL) antibody of IgG and/or IgM isotype in serum or plasma, present in medium or high titer, on two or more occasions, at least 12 weeks apart.
- Anti-β2 glycoprotein-I antibody of IgG and/or IgM isotype in serum or plasma, present on two or more occasions, at least 12 weeks apart.
*Classification of APS should be avoided if less than 12 weeks or more than 5 years separate the positive aPL test and the clinical manifestation.
Reference:
International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost 2006.
Differential diagnosis
The differential diagnosis should include other diseases or procoagulation states that increase the risk of thrombosis, for example: protein C deficiency, protein S deficiency or antithrombin III deficiency, dysfibrinogenaemia, increased activity of coagulation factor IX, XI or VIII, paroxysmal nocturnal haemoglobinuria, homocystinuria, malignancy, oral contraceptive.
In the case of pregnancy loss, other causes of recurrent miscarriage have to be excluded, for example: genetic abnormalities, uterine anomalies, cervical incompetence or infections.
Treatment
Although there is no cure, a correct diagnosis and treatment could greatly reduce the risk of developing blood clots and miscarriages.
Oral anticoagulation with vitamin K antagonists (VKAs) is the cornerstone of the treatment of thrombotic APS. Other anticoagulants, such as low molecular weight heparin (LMWH), should be used in high-risk situations such as surgery, prolonged immobilization, pregnancy with recurrent miscarriages or pregnant women with a history of thrombotic event and the puerperium.
In certain cases, low dose aspirin could be used as a measure to prevent thrombosis (e.g. aPL carriers (high profile) without previous events).
Nevertheless, general measures for aPL-positive individuals should include screening for and strict control of cardiovascular risk factors (smoking cessation; management of hypertension, dyslipidemia and diabetes; and regular physical activity).
Prognosis
The severity of APS varies from person to person, so the prognosis is also variable. APS can cause life-threatening or life-limiting illnesses – depending on the location and the extent of the thrombosis. In rare instances, a catastrophic APS supervenes. A higher risk of recurrent thrombosis is associated with the presence of lupus anticoagulant and/ triple antiphospholipid antibodies positivity (i.e. positivity for lupus anticoagulant, anti-cardiolipin and anti-β2glycoprotein I antibodies), as opposed to a positive result of only one test. (Reference: Hernández-Molina, et al. The role of lupus anticoagulant and triple marker positivity as risk factors for rethrombosis in patients with primary antiphospholipid syndrome. Clin Exp Rheumatol,. 2013). Long-term anticoagulation does seem to improve prognosis in APS. With the appropriate medication and a healthy lifestyle, most people with primary APS can lead a normal healthy life.
Women with antiphospholipid syndrome can give birth to a healthy baby if they follow their doctor’s instructions and take medication regularly.
APS as a secondary CTD
APS may be associated with other autoimmune diseases – Secondary APS. Majority of the cases occur in association with systemic lupus erythematosus (SLE). The clinical features and management of SLE-associated APS are similar to those of primary APS.
Pregnancy planning
APS can cause complications during pregnancy, for example:
- Repeated miscarriages
- Intrauterine growth restriction, which happens when a baby in the womb grows slower than expected
- Preeclampsia, or high blood pressure during pregnancy
- Eclampsia, a life threatening complication of preeclampsia
- Stillbirth
Moreover, patients with APS are more prone to blood clots during pregnancy and up to 6 weeks after pregnancy.
It is crucial for all women with APS to have pre pregnancy counseling with their partner to discuss their future management in pregnancy management and define their specific risks. In case of confirmed pregnancy women should be referred to their obstetrician and rheumatologist as early as possible to assess the state of their health and to decide on the need for treatment with aspirin or heparin. Women who take warfarin should switch to anticoagulation with low-dose aspirin and heparin as soon as pregnancy is confirmed, ideally before week 6 of gestation, because of the teratogenic effects of warfarin.
Once pregnancy is achieved, frequent office visits will be needed to:
- Blood and urine tests
- Blood pressure measurements
- Obstetrical ultrasound examinations (more frequently during the third trimester)
In the postnatal period, women who were previously been receiving warfarin may restart warfarin and discontinue heparin. It is safe for the neonate to breastfeed while the mother is taking either heparin or warfarin.
Reference:
Andreoli L, et al.; EULAR recommendations for women’s health and the management of family planning, assisted reproduction, pregnancy and menopause in patients with systemic lupus erythematosus and/or antiphospholipid syndrome; Annals of the Rheumatic Diseases 2017.
APS in children
APS can start in childhood. APS can be diagnosed alone in children or can be associated with other CTD, primarily Systemic Lupus Erythematosus. Although the estimated prevalence (2.5/100,000 people) [Ref 1] is relatively low, recurrent clinical manifestations and catastrophic APS are relatively high in children with APS. Evaluation by a specialist is fundamental to avoid diagnostic delay and to prevent damage in children with suspected APS. Evaluation and follow-up at a dedicated pediatric rheumatology supported by a multidisciplinary team are essential.
Coping and support for patients
The experience of chronic disease needs adaptation in multiple life domains. We recommend that you discuss your fears and doubts with your health team along the way.
To improve the quality of life in chronic disease, consider the following:
- Social support – identify patient associations dedicated to APS. Connect to patients who are more advanced in their adjustment. But remember that every person has their own adaptation time and personality!
- Social rights – learn about the social rights you have in your country, including the ones regarding adjustments at the workplace
- Support of family and friends. They should be educated in the matters of your disease and your needs to be able to support you. They often feel lost and are misinformed
- Be part of your community
Psychological Health
Chronic diseases carry important psychological and social consequences that demand significant psychological adjustment.
Don’t be scared to address these issues with your doctors or other health professionals. You may experience the effects of this chronic disease on one’s sense of self.
To improve your psychological health, consider the following:
- Professional help: psychological support, patient support groups, and psychotherapy. Be aware of your needs, anxiety, or depression, and ask for psychological evaluation
- Programs/courses of psychological health in chronic patients with your disease or similar in order to develop coping skills, mindfulness, communication, reduce stress or meditation
- Educational materials, webinars, and courses on the disease
- Learn to communicate your symptoms and needs – you are the expert on what you feel. You need to be in control of your life, your decisions, and the person you want to be. You are not a disease; you are a person with a disease
Lifestyle tips
– Avoid being overweight:
- Have a balanced and healthy diet – for more info, please click here
- Consume less salt, saturated fats and sugar
- Exercise regularly – at least 150 minutes a week of moderate-intensity physical activity (30 minutes per day)
– Quit smoking
– Reduce alcohol consumption
– Get vaccinated
– Women should avoid using estrogen therapy for contraception or menopause
– If you take blood-thinning medications:
- You should avoid situations where you could be injured or fall
- Use a soft toothbrush
- Shave with an electric razor
- Be careful when using sharp tools like knives
- See your healthcare provider regularly to monitor your treatment
– Stay engaged with your community
– Have a work and family life balance
– Talk about your sexuality issues with your medical team
– Do something you feel passionate about
Useful links:
- Related ERN ReCONNET webinars can be seen in this webpage
- Congresses with patient participation, Other events (will be uploaded soon)
How to prepare for the doctor’s visit
- Arrive early, as you may need to complete forms
- Clarify what your main symptoms are. Think about your complaints and try to describe them as best you can. If you are a new patient, you can compile a diary/list with your complaints and other health problems.
- Be prepared to share your medical history and that of your family members. Doctors will ask you for this informations at the first visit. You can write down: when your symptoms began, how the symptoms changed over time, previous doctor visits and tests, any treatment that have been tried
- Bring all prior medical documents (tests, letters, X-rays, etc.)
- Bring a list of the medicines you take. Remember the side effects of relevant current or prior medications
- Remember to tell your doctor other details about your health, such as vaccination schedules, allergies, and family health history
- Bring a family member if you are nervous and afraid you could miss discussion points during your appointment
- At the end of the consultation, make a note of your next appointment and ask how to proceed if you have an urgent health problem or cannot tolerate the medication
Diagnostic path
- Find the Medical Center – Please check the ERN ReCONNET centers list below
- Medical interview with a doctor – Please check the paragrah above: How to prepare for a Doctor visit
- The doctor may refer you for lab tests, in particular testing for antiphospholipid antibodies and other tests (Doppler ultrasound exam, X-rays, etc.), or other specialists. You will have a follow-up visit after collecting all the necessary test results and medical consultations
- At the follow-up visit, the doctor may confirm a suspected diagnosis, refer for more tests or rule out a suspected diagnosis
- Once the diagnosis is established, the doctor will discuss further treatment with you
- Since the disease is chronic, it is essential to visit your doctor regularly and perform check-up exams routinely as prescribed by a specialisT
 Here is a list of APS patient associations
Here is a list of APS patient associations
Other groups
Italy. Feder-A.I.P.A. and Lupus Italy
Spain. SAF España
UK. APS Support
LIST OF USEFUL REFERENCES
- New APS Classification Criteria Collaborators. Development of a New International Antiphospholipid Syndrome Classification Criteria Phase I/II Report: Generation and Reduction of Candidate Criteria
Barbhaiya M, Zuily S, Ahmadzadeh Y, Amigo MC, Avcin T, Bertolaccini ML, Branch DW, de Jesus G, Devreese KMJ, Frances C, Garcia D, Guillemin F, Levine SR, Levy RA, Lockshin MD, Ortel TL, Seshan SV, Tektonidou M, Wahl D, Willis R, Naden R, Costenbader K, Erkan D; New APS Classification Criteria Collaborators.
Arthritis Care Res (Hoboken). 2021 Oct;73(10):1490-1501.
- Use of Direct Oral Anticoagulants in Patients With Antiphospholipid Syndrome: A Systematic Review and Comparison of the International Guidelines
Pastori D, Menichelli D, Cammisotto V, Pignatelli P.
Front Cardiovasc Med. 2021 Aug 3;8:715878.
- 16th International congress on antiphospholipid antibodies task force report on clinical manifestations of antiphospholipid syndrome
Sciascia S, Radin M, Cecchi I, Levy RA, Erkan D.
Lupus. 2021 Jul;30(8):1314-1326.
- EULAR recommendations for the management of antiphospholipid syndrome in adults
Tektonidou MG, Andreoli L, Limper M, Amoura Z, Cervera R, Costedoat-Chalumeau N, et al.
Ann Rheum Dis. 2019;78:1296-1304.
- European evidence-based recommendations for diagnosis and treatment of childhood-onset systemic lupus erythematosus: the SHARE initiative
Groot N, Graeff N de, Avcin T, Bader-Meunier B, Brogan P, Dolezalova P, et al.
Ann Rheum Dis. 2017 Nov;76(11):1788-1796.
- European evidence-based recommendations for diagnosis and treatment of paediatric antiphospholipid syndrome: the SHARE initiative
Groot N, de Graeff N, Avcin T, Bader-Meunier B, Dolezalova P, Feldman B, et al.
Ann Rheum Dis. 2017 Oct;76(10):1637-1641.
- EULAR recommendations for women’s health and the management of family planning, assisted reproduction, pregnancy and menopause in patients with systemic lupus erythematosus and/or antiphospholipid syndrome
Andreoli L, Bertsias GK, Agmon-Levin N, Brown S, Cervera R, Costedoat-Chalumeau N, et al.
Ann Rheum Dis. 2017 Mar;76(3):476-485.
- Pregnancy loss: French clinical practice guidelines
Huchon C, Deffieux X, Beucher G, Capmas P, Carcopino X, Costedoat-Chalumeau N, et al.
Eur J Obstet Gynecol Reprod Biol. 2016 Jun;201:18-26.
- Guidelines on the investigation and management of antiphospholipid syndrome
Keeling D, Mackie I, Moore GW, Greer IA, Greaves M.
Br J Haematol. 2012 Apr;157(1):47-58.
- VTE, Thrombophilia, Antithrombotic Therapy, and Pregnancy : Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines
Bates SM, Greer IA, Middeldorp S, Veenstra DL, Prabulos A-M, Vandvik PO.
Chest. 2012 Feb;141(2):e691S-e736S.
- International consensus guidelines on anticardiolipin and anti-fl 2-glycoprotein i testing: Report from the 13th International Congress on Antiphospholipid Antibodies
Lakos G, Favaloro EJ, Harris EN, Meroni PL, Tincani A, Wong RC, et al.
Arthritis Rheum. 2012 Jan;64(1):1-10.
- Evidence-based recommendations for the prevention and long-term management of thrombosis in antiphospholipid antibody-positive patients: report of a task force at the 13th International Congress on antiphospholipid antibodies
Ruiz-Irastorza G, Cuadrado MJ, Ruiz-Arruza I, Brey R, Crowther M, Derksen R, et al.
Lupus. 2011 Feb;20(2):206-18.
- EULAR recommendations for the management of systemic lupus erythematosus with neuropsychiatric manifestations: report of a task force of the EULAR standing committee for clinical affairs
Bertsias GK, Ioannidis JPA, Aringer M, Bollen E, Bombardieri S, Bruce IN, et al.
Ann Rheum Dis. 2010 Dec;69(12):2074-82.
- Update of the guidelines for lupus anticoagulant detection
Pengo V, Tripodi A, Reber G, Rand JH, Ortel TL, Galli M, et al.
J Thromb Haemost. 2009 Oct;7(10):1737-40.
- EULAR recommendations for the management of systemic lupus erythematosus. Report of a Task Force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics
Bertsias G, Ioannidis JPA, Boletis J, Bombardieri S, Cervera R, Dostal C, et al.
Ann Rheum Dis. 2008 Feb;67(2):195-205.
- Venous thromboembolism in the antiphospholipid syndrome: management guidelines for secondary prophylaxis
Meroni PL, Moia M, Derksen RH, Tincani A, McIntyre JA, Arnout JM, et al.
Lupus. 2003;12(7):504-7.
- Catastrophic antiphospholipid syndrome: international consensus statement on classication criteria and treatment guidelines
Asherson RA, Cervera R, de Groot PG, Erkan D, Boffa MC, Piette JC, et al.
Lupus. 2003;12(7):530-4.
Barbhaiya M, Zuily S, Ahmadzadeh Y, Amigo MC, Avcin T, Bertolaccini ML, Branch DW, de Jesus G, Devreese KMJ, Frances C, Garcia D, Guillemin F, Levine SR, Levy RA, Lockshin MD, Ortel TL, Seshan SV, Tektonidou M, Wahl D, Willis R, Naden R, Costenbader K, Erkan D; New APS Classification Criteria Collaborators.
Arthritis Care Res (Hoboken). 2021 Oct;73(10):1490-1501.
Pastori D, Menichelli D, Cammisotto V, Pignatelli P.
Front Cardiovasc Med. 2021 Aug 3;8:715878.
Sciascia S, Radin M, Cecchi I, Levy RA, Erkan D.
Lupus. 2021 Jul;30(8):1314-1326.
Tektonidou MG, Andreoli L, Limper M, Amoura Z, Cervera R, Costedoat-Chalumeau N, et al.
Ann Rheum Dis. 2019;78:1296-1304.
Groot N, Graeff N de, Avcin T, Bader-Meunier B, Brogan P, Dolezalova P, et al.
Ann Rheum Dis. 2017 Nov;76(11):1788-1796.
Groot N, de Graeff N, Avcin T, Bader-Meunier B, Dolezalova P, Feldman B, et al.
Ann Rheum Dis. 2017 Oct;76(10):1637-1641.
Andreoli L, Bertsias GK, Agmon-Levin N, Brown S, Cervera R, Costedoat-Chalumeau N, et al.
Ann Rheum Dis. 2017 Mar;76(3):476-485.
Huchon C, Deffieux X, Beucher G, Capmas P, Carcopino X, Costedoat-Chalumeau N, et al.
Eur J Obstet Gynecol Reprod Biol. 2016 Jun;201:18-26.
Keeling D, Mackie I, Moore GW, Greer IA, Greaves M.
Br J Haematol. 2012 Apr;157(1):47-58.
Bates SM, Greer IA, Middeldorp S, Veenstra DL, Prabulos A-M, Vandvik PO.
Chest. 2012 Feb;141(2):e691S-e736S.
Lakos G, Favaloro EJ, Harris EN, Meroni PL, Tincani A, Wong RC, et al.
Arthritis Rheum. 2012 Jan;64(1):1-10.
Ruiz-Irastorza G, Cuadrado MJ, Ruiz-Arruza I, Brey R, Crowther M, Derksen R, et al.
Lupus. 2011 Feb;20(2):206-18.
Bertsias GK, Ioannidis JPA, Aringer M, Bollen E, Bombardieri S, Bruce IN, et al.
Ann Rheum Dis. 2010 Dec;69(12):2074-82.
Pengo V, Tripodi A, Reber G, Rand JH, Ortel TL, Galli M, et al.
J Thromb Haemost. 2009 Oct;7(10):1737-40.
Bertsias G, Ioannidis JPA, Boletis J, Bombardieri S, Cervera R, Dostal C, et al.
Ann Rheum Dis. 2008 Feb;67(2):195-205.
Meroni PL, Moia M, Derksen RH, Tincani A, McIntyre JA, Arnout JM, et al.
Lupus. 2003;12(7):504-7.
Asherson RA, Cervera R, de Groot PG, Erkan D, Boffa MC, Piette JC, et al.
Lupus. 2003;12(7):530-4.
- Update on Antiphospholipid Syndrome: Ten Topics in 2017
Cavazzana I, Andreoli L, Limper M, Franceschini F, Tincani A.
Curr Rheumatol Rep. 2018 Mar 15;20(3):15.
- Antiphospholipid syndrome: an update for clinicians and scientists
Vreede AP, Bockenstedt PL, Knight JS.
Curr Opin Rheumatol. 2017 Sep;29(5):458-466.
- Mechanisms of thrombosis in systemic lupus erythematosus and antiphospholipid syndrome
de Groot PG, de Laat B.
Best Pract Res Clin Rheumatol. 2017 Jun;31(3):334-341.
- Antiphospholipid syndrome
Cervera R.
Thromb Res. 2017 Mar;151 Suppl 1:S43-S47.
- Pregnancy and Antiphospholipid Syndrome
Schreiber K, Hunt BJ.
Semin Thromb Hemost. 2016 Oct;42(7):780-788.
- The relevance of “non-criteria” clinical manifestations of antiphospholipid syndrome: 14th International Congress on Antiphospholipid Antibodies Technical Task Force Report on Antiphospholipid Syndrome Clinical Features
Abreu MM, Danowski A, Wahl DG, Amigo MC, Tektonidou M, Pacheco MS, et al.
Autoimmun Rev. 2015 May;14(5):401-14.
- 14th International Congress on Antiphospholipid Antibodies Task Force. Report on antiphospholipid syndrome laboratory diagnostics and trends
Bertolaccini ML, Amengual O, Andreoli L, Atsumi T, Chighizola CB, Forastiero R, et al.
Autoimmun Rev. 2014 Sep;13(9):917-30.
- 14th International Congress on Antiphospholipid Antibodies Task Force report on obstetric antiphospholipid syndrome
de Jesus GR, Agmon-Levin N, Andrade CA, Andreoli L, Chighizola CB, Porter TF, Salmon J, Silver RM, Tincani A, Branch DW.
Autoimmun Rev. 2014 Aug;13(8):795-813.
- Evidence based treatment of the antiphospholipid syndrome II. Optimal anticoagulant therapy for thrombosis
Crowther MA, Wisloff F.
Thromb Res. 2005;115(1-2):3-8.
- Prophylaxis of the antiphospholipid syndrome: a consensus report
Alarcón-Segovia D, Boffa MC, Branch W, Cervera R, Gharavi A, Khamashta M, et al.
Lupus. 2003;12(7):499-503.
Cavazzana I, Andreoli L, Limper M, Franceschini F, Tincani A.
Curr Rheumatol Rep. 2018 Mar 15;20(3):15.
Vreede AP, Bockenstedt PL, Knight JS.
Curr Opin Rheumatol. 2017 Sep;29(5):458-466.
de Groot PG, de Laat B.
Best Pract Res Clin Rheumatol. 2017 Jun;31(3):334-341.
Cervera R.
Thromb Res. 2017 Mar;151 Suppl 1:S43-S47.
Schreiber K, Hunt BJ.
Semin Thromb Hemost. 2016 Oct;42(7):780-788.
Abreu MM, Danowski A, Wahl DG, Amigo MC, Tektonidou M, Pacheco MS, et al.
Autoimmun Rev. 2015 May;14(5):401-14.
Bertolaccini ML, Amengual O, Andreoli L, Atsumi T, Chighizola CB, Forastiero R, et al.
Autoimmun Rev. 2014 Sep;13(9):917-30.
de Jesus GR, Agmon-Levin N, Andrade CA, Andreoli L, Chighizola CB, Porter TF, Salmon J, Silver RM, Tincani A, Branch DW.
Autoimmun Rev. 2014 Aug;13(8):795-813.
Crowther MA, Wisloff F.
Thromb Res. 2005;115(1-2):3-8.
Alarcón-Segovia D, Boffa MC, Branch W, Cervera R, Gharavi A, Khamashta M, et al.
Lupus. 2003;12(7):499-503.
APS centres in ERN ReCONNET
- Civil Hospital – Brescia
- AOU Meyer di Firenze (paediatric)
- ASST Centro Specialistico Ortopedico Traumatologico Gaetano Pini (Presidio Pini)
- AO Padua
- AOU Pisan
- AOU Policlinico Umberto I di Roma
- Fondazione Policlinico Tor Vergata Roma
- AOU S. Giovanni di Dio e Ruggi D’Aragona
- A.S.L. Torino – Hub S. Giovanni Bosco
- Azienda Ospedaliera Universitaria Integrata di Verona
- University Medical Centre Ljubljana (paediatric)




