ERN ReCONNET
Disease Info
Disease: Undifferentiated Connective Tissue Disease
Undifferentiated Connective Tissue Disease (UCTD)
Overview – What is UCTD?
Undifferentiated connective tissue disease (UCTD) is a rare autoimmune clinical entity defined by the presence of serological and clinical manifestations often seen in association with systemic autoimmune diseases (SAD) but not extensive or specific enough to fulfill any criteria of defined connective tissue disease (CTD) such as systemic sclerosis (SSc), systemic lupus erythematosus (SLE), mixed connective tissue disease, Sjögren’s syndrome, polymyositis, dermatomyositis, or rheumatoid arthritis (RA). Although the term “undifferentiated” sounds vague, it describes a real problem and one that is quite common in rheumatology practice. It does not mean that a doctor does not know how to call the condition; it just means that specific features traditionally seen in defined connective tissue disease are absent.
Epidemiology
Over 90% of patients are female, between 30 and 45 years old.
The estimated annual incidence is 40-150 per 100000 adults.
Causes
The cause of UCTD is not entirely understood. It is believed that genetic and environmental factors (such as infections, chemicals found in cigarette smoke, air pollutants, or UV light) play a significant role in developing the disease.
The estimated annual incidence is 40-150 per 100000 adults.
Luca Iaccarino
Luca Iaccarino
Disease Coordinator
Disease Coordinator
Ramona Luciu
Ramona Luciu
ePAG representative
ePAG representative
Cristina Pamfil
Cristina Pamfil
Disease Coordinator
Disease Coordinator
Vera Guimarães
Vera Guimarães
ePAG representative
(ad interim)
ePAG representative
(ad interim)

Raynaud’s phenomenon
Common symptoms
Joints:
- Arthralgia (up to 86%) – joint pain mostly early in the morning / during the night
- Arthritis (joint inflammation – tender, warm, and swollen joints) (22%)
- Prolonged morning stiffness – painful and limited joint mobility
Skin lesions:
- Raynaud’s phenomenon (around 33%)
- Livedo reticularis – a mottled reticulated vascular pattern that appears as a lace-like purplish discoloration of the skin
- Purpura – purple or red spots on the skin, especially on the lower limbs
- Acrocyanosis – persistent blue or cyanotic discoloration of the extremities, most commonly occurring in the hands, although it also occurs in the feet and distal parts of the face (ears, nose, lips)
- Telangiectasia – small dilated blood vessels located near the surface of the skin or mucous membranes
- Sun-sensitive rash – on sun-exposed areas, such as the face, neck, or anterior upper chest
- Hair loss – usually mild, in some cases may progress to partial or complete baldness
- Sclerodactyly – thickening and tightness of the skin of the fingers or toes
Eyes:
- Dry eyes (30%) – decreased production of tears leading to itching, redness, pain, and the feeling of sand in the eyes
- Uveitis – inflammation of the uvea, the pigmented layer of the eye, usually manifested as pain and redness of one eye with increased sensitivity to light and hyperlacrimation
- Conjunctivitis
Thyroid disease (7%)
Lungs:
- Pleuritis – inflammation of the pleura
- Interstitial lung disease – manifested as cough, shortness of breath, or flu-like symptoms
Heart:
- Pericarditis – inflammation of the pericardium around the heart
- Irregular heartbeat
- Cardiomegaly – enlarged heart
Gastrointestinal:
- Oral ulcers (23%) – sores inside the mouth
- Dry mouth (30%) – decreased production of saliva
- Splenomegaly – enlarged spleen
- Hepatomegaly – enlarged liver
- Abdominal tenderness
WEBINARS
Genitalia:
- Ulcerations
Muscles:
- Myalgia – pain in the muscles
- Muscles weakness
Hematological disorders:
- Anemia – low red blood cells count or low hemoglobin
- Leukopenia – low white blood cell count
- Thrombocytopenia – low platelet count (manifested as easy bruising, gum bleeding)
Neurological disorders:
- Peripheral neuropathy – abnormal nerve sensations in limbs
Fever (15%)
Fatigue – tiredness, lack of energy and motivation
What is Raynaud’s phenomenon and how to manage it?
Raynaud’s phenomenon (RP) can be primary (on its own) or secondary (along with other diseases like SLE, SSc, or UCTD). RP results from prolonged vasoconstriction of the small vessels causing decreased blood flow to the fingers, rarely toes, usually provoked by cold, stress, or emotional upset.
RP manifests as white-pale, blue, and red fingers with pins and needles sensations, discomfort, and pain. The symptoms resolve spontaneously. In severe cases of secondary RP, prolonged vasoconstriction can lead to digital ulceration or gangrene.
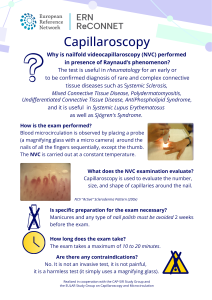
The diagnosis is established based on the patient’s history and physical examination. Usually, the doctor performs nailfold capillaroscopy to examine the blood vessels below the fingernails.
General recommendations for RP:
- Keep the body warm and avoid exposure to cold and sudden temperature changes. Try not to go quickly from heat to air conditioning
- Manage stress. Stress can trigger Raynaud’s symptoms
- Quit smoking, but also avoid passive smoking! Smoke causes skin temperature to drop
- Avoid hand injuries. In patients with RP, hand injuries can take longer to heal
- Exercise. Exercise increases blood flow
During an RP attack:
- Immediately get indoors or to a warmer area
- Massage your hands and feet
- Wiggle your fingers and toes
- Place your hands under your armpits or un your warm belly
- Make wide circles with your arms
- Run warm (not hot!) water over your fingers and toes
When to see a doctor?
If you develop any of the symptoms above, make an appointment with your GP, especially if they are severe, persistent, and recurrent. He can refer you to a specialist, such as a rheumatologist.
Once you have a diagnosis established, the rheumatologist may schedule regular visits. However, make another appointment if your symptoms worsen or you develop new symptoms.
How to prepare for the doctor’s visit
- Arrive early, as you may need to complete forms
- Clarify what your main symptoms are. Think about your complaints and try to describe them as best you can. If you are a new patient, you can compile a diary/list with your complaints and other health problems
- Bring all prior medical documents (tests, letters, X-rays, etc.)
- Bring a list of the medicines you take. Remember the side effects of relevant current or prior medications
- Remember to tell your doctor other details about your health, such as vaccination schedules, allergies, and family health history
- Bring a family member if you are nervous and afraid you could miss discussion points during your appointment
- At the end of the consultation, make a note of your next appointment and ask how to proceed if you have an urgent health problem or cannot tolerate the medication
Diagnostic path
- Find the Medical Center – Click here (A map of ReCONNET centers)
- Medical interview with a doctor – Click here (How to prepare for a Doctor visit)
- The doctor may refer you for lab tests, other tests (ultrasound, X-rays, etc.), or other specialists
- You will have a follow-up visit after collecting all the necessary test results and medical consultations
- At the follow-up visit, the doctor may confirm a suspected diagnosis, refer for more tests or rule out a suspected diagnosis
- Once the diagnosis is established, the doctor will discuss further treatment with you
- Since the disease can evolve into a defined connective tissue disease, it is essential to visit your doctor regularly
Diagnostics tests (below you will find some of the tests that are needed to better understand the clinical picture)
Blood tests:
- ANA – antinuclear antibodies
- Complete blood count
- C-reactive protein (CRP)
- Erythrocyte sedimentation rate (ESR)
- Serum creatinine, liver function tests, muscle enzymes
- Urinalysis with microscopic analysis
- Rheumatoid factor (RF)
- Other tests (protein electrophoresis, complement C3 and C4, anti-CCP antibodies)
Imaging studies:
- X-rays
- Ultrasounds
- Other tests
Other tests, for example:
- Pulmonary function tests
- Echocardiography
- Schirmer’s test
- Nailfold capillaroscopy
Meaning of antinuclear antibodies (ANA)
Antinuclear antibodies (ANA) are autoantibodies directed against human cell components. The detection of ANA is the first screening test performed when an autoimmune disease is hypothesized. A positive ANA test means autoantibodies are present in the patient’s blood. ANA can be positive in healthy individuals (3-15% cases), and their incidence increases in individuals over 65. Also, certain medications and other conditions, such as cancer and infections, can affect the test result. Like autoimmunity itself, ANA expression is more common among women than men. To verify the result of the ANA test, the doctor will carry out several other blood tests and correlate them with your symptoms and medical history. Keep in mind that antinuclear antibodies may be detected before clinical manifestations. ANA are detected with a fluorescent test, and the fluorescence pattern may be evocative of a specific antigen positivity which is more informative about the potential underlying disease. Anti-Ro/SSA and anti-U1-RNP, the most frequently encountered ANA subtypes in UCTD, are detected using a second-level blood test. In UCTD, the autoantibody profile remains stable over time, and new autoantibody specificities are rare and usually observed in those patients who will evolve to defined CTDs.
Classification criteria
Due to the heterogeneity of disease manifestations of connective tissue diseases, no diagnostic criteria have been established to date. A patient can be classified into a group of patients who share UCTD features if they have persisting signs and symptoms suggestive of a CTD for at least three years but do not meet the criteria for definite CTD and have positive antinuclear antibodies on two separate measurements.
Differential diagnosis
UCTD is a diagnosis of exclusion; therefore, it is necessary to consider defined connective tissue diseases, especially the “early phase” of defined CTDs.
Treatment
UCTD usually requires only mild therapeutic intervention. The treatment is tailored according to disease manifestations and could include:
- Nonsteroidal anti-inflammatory drugs like naproxen, celecoxib, etc. – to control musculoskeletal pain and inflammation
- Glucocorticoids – used to induce remission in case of flare-up
- Immunosuppressant agents like methotrexate or azathioprine – to control severe symptoms
- Antimalarial drugs (ex. hydroxychloroquine) – usually in case of skin rashes, photosensitivity, or articular symptoms
- Calcium channel blockers like amlodipine or nifedipine – in the case of Raynaud’s phenomenon
- Sunblock lotions
- Protective measures in case of exposure to cold
Prognosis
- Most of the patients have a mild clinical course
- Most people with UCTD do not develop major organ damage (such as problems with the kidneys, liver, heart, lungs, or brain) or life-threatening disease
- Up to 40% of patients with UCTD may evolve a defined CTD within 3-5 years
- Around 25% of patients can experience the complete remission of symptoms
- Among the patients who evolve into a defined CTD, SLE is the most common
UCTD as the early stage of defined CTD
Up to 40% of patients with UCTD may evolve into a defined CTD within 3-5 years. Follow-up visits are essential, especially during the first years from symptoms onset, because they allow the physician to monitor clinical manifestations and reevaluate the diagnosis. The progression into a defined CTD is more likely when the patient has specific symptoms for a CTD, called red flags.
Red flags for progression to SLE are younger age, serositis, malar rash, renal involvement, the presence of specific antibodies (anti-Sm, anti-dsDNA), or hypocomplementemia.
Red flags for progression to SSc are persistent Raynaud’s phenomenon, puffy fingers, SSc-specific autoantibodies (anticentromere, anti-topoisomerase I, anti-RNA polymerase III), and a scleroderma pattern in nailfold capillaroscopy.
Pregnancy planning
UCTD is the most frequently diagnosed CTD during the first trimester of pregnancy. Patients who become pregnant in a moment of high disease activity have an increased risk of progression into defined CTD, disease flares (moments of increased symptoms), and obstetric complications. Miscarriages and pre-term deliveries are the most frequently obstetric complications described in up to 20% of patients; severe obstetric complications are rare (preeclampsia 1-2%, severe growth restriction <1%, intrauterine fetal death <1%) and similar to the general population.
On the other hand, controlling the disease activity (remission) before conception and during pregnancy ensures good outcomes for both mother and baby.
Pregnant women with UCTD require careful monitoring since 3-12% will develop a defined connective tissue disease by the end of pregnancy. The risk of progression to SLE is increased in persons with positive anti-dsDNA antibodies.
Women with UCTD should be in the care of a tertiary pregnancy center with a specialized multidisciplinary team of rheumatologists and obstetricians. Preconception counseling, pregnancy planning, and monitoring are mandatory to ensure the best outcome. Importantly, women who wish to conceive should be tested for specific antibodies (anti-Ro, aPL antibodies) to determine the risk of possible adverse outcomes in order to plan for specific therapeutic strategies and monitoring. Pregnant women should promptly inform doctors about new signs and symptoms.
Treatment of UCTD in pregnancy:
- Hydroxychloroquine is safe during pregnancy and breastfeeding
- Azathioprine and cyclosporine are safe during pregnancy and breastfeeding
- Methotrexate (MTX), mycophenolate mofetil (MMF), and leflunomide are contraindicated in pregnancy. MMF should be discontinued six weeks and MTX three months before pregnancy, respectively
- Nonsteroidal anti-inflammatory drugs, except for low-dose aspirin, should be avoided in the third trimester
- Low-dose glucocorticoids are safe during pregnancy and breastfeeding. Some guidelines recommend waiting up to 4 hours before breastfeeding after the maternal dose of an oral corticosteroid to decrease the potential exposure of the infant
UCTD in children
UCTD can start in childhood. Raynaud’s phenomenon may be the first symptom, and in fact, ~10% of children with Raynaud’s phenomenon will be diagnosed with UCTD. Evaluation and follow-up at a dedicated pediatric rheumatology are essential. Symptoms such as joint pain may be difficult to assess in children, and a careful approach is fundamental.
Coping and support for patients
The experience of chronic disease needs adaptation in multiple life domains. As a patient, we recommend that you discuss your fears and doubts with your health team along the way.
To improve the quality of life in chronic disease, consider the following:
- Social support – identify patient associations dedicated to rheumatic diseases. Connect to patients who are more advanced in their adjustment But remember that every person has their own adaptation time and personality!
- Social rights – learn about the social rights you have in your country, including the ones regarding adjustments at the workplace
- Support of family and friends. They should be educated in the matters of your disease and your needs to be able to support you. Often, they feel lost and are misinformed
- Be part of your community
Psychological Health
Chronic diseases carry important psychological and social consequences that demand significant psychological adjustment. Don’t be scared to address these issues with your doctors or other health professionals. You may experience the effects of this chronic disease on one’s sense of self.
To improve your psychological health, consider the following:
- Professional help: psychological support, patient support groups, and psychotherapy. Be aware of your needs, humor changes, anxiety, or depression, and ask for psychological evaluation
- Programs/courses of psychological health in chronic patients with your disease or similar in order to develop coping skills, mindfulness, communication, reduce stress or meditation
- Educational materials, webinars, and courses on the disease (it is not easy to find specific material for UCTD)
- Learn to communicate your symptoms and needs – you are the expert on what you feel. You need to be in control of your life, your decisions, and the person you want to be. You are not a disease; you are a person with a disease
Lifestyle tips
- Have a balanced and healthy diet – for more: https://www.who.int/europe/news-room/fact-sheets/item/a-healthy-lifestyle—who-recommendations
- Consume less salt and sugar
- Exercise regularly – at least 150 minutes a week of moderate-intensity physical activity (30 minutes per day)
- Ensure good quality sleep – for more: https://www.sleepfoundation.org/sleep-hygiene
- Quit smoking
- Reduce alcohol consumption
- Get vaccinated
- Do something you feel passionate about
- Stay engaged with your community
- Have a work and family life balance
- Talk about your sexuality issues with your medical team
A list of patient associations can be found here.
Blog about UCTD
ERN RECONNET PUBLICATIONS ARE AVAILABLE FOR CONSULTATION.
List of useful references
- Undifferentiated connective tissue disease: state of the art on clinical practice guidelines. Antunes et al., RMD Open. 2019.
- The diagnosis and classification of undifferentiated connective tissue diseases. Mosca M. et al., Autoimmun. 2014.
- UCTD preliminary classification criteria. Mosca M. et al., Clin Exp Rheumatol. 1999.
- Undifferentiated Connective Tissue Disease. Marwa K. and Anjum F., STATPearls, 2023.
- What‘s causing your pain?
- EULAR PARE: Physical activity at home for people with RMDs
- Undifferentiated Connective Tissue Disease in Pregnancy: A Topic Yet to be Explored. Serena C. et al., Frontiers in Pharmacology. 2022.
- Pregnancy and undifferentiated connective tissue disease: Outcome and risk of flare in 100 pregnancies. Zucchi D. et al., Rheumatology, 2020,
- Predicting progression from undifferentiated connective tissue disease to definite connective tissue disease: A systematic review and meta-analysis. Dyball S. et al., Autoimmunity Reviews. 2022.
- The Psychosocial Impact of UCTD on Patient Health and Well-Being: A Qualitative Study. Siegel C. et al., JCR: Journal of Clinical Rheumatology. 2022.
- Clinical Significance of Antinucleolar Antibodies. Minoru Satoh M. et al., Clinical Reviews in Allergy & Immunology. 2022.
UCTD centres in ERN ReCONNET
Helsinki University Hospital, Hospital District of Helsinki and Uusimaa, Finland (ReCONNETFIN) (adult and paedriatric)
- Civil Hospital – Brescia
- AOU Careggi, Florence
- AOU Meyer di Firenze (paediatric)
- IRCCS AOU San Martino – Genoa
- Foundation IRCCS CA’Granda Ospedale Maggiore polyclinic – Milan
- ASST Centro Specialistico Ortopedico Traumatologico Gaetano Pini (Presidio Pini)
- AO Padua
- Foundation IRCCS Polyclinic San Matteo, Pavia
- AOU Pisan
- AOU Policlinico Umberto I di Roma
- Fondazione Policlinico Tor Vergata Roma
- A.S.L. Torino – Hub S. Giovanni Bosco
- Azienda Ospedaliera Universitaria Integrata di Verona
- Hospital Clínic de Barcelona y Hospital de Sant Joan de Déu (adult and paediatric)
- Hospital Universitario 12 de Octubre