ERN ReCONNET
Disease Info
Disease: Mixed Connective Tissue Disease
Mixed Connective Tissue Disease (MCTD)
Overview – What is MCTD?
Clinical overview of the disease
Mixed connective tissue disease (MCTD) is a rare autoimmune disease. MCTD is characterized by overlapping features of various systemic connective tissue diseases, including systemic lupus erythematosus (SLE), systemic sclerosis (SSc), dermato-/polymyositis (DM/PM), and rheumatoid arthritis (RA). Typical is the presence of antibodies against U1-ribonucleoprotein, especially in high titers. In the clinical picture, symptoms from different systems and organs are observed and they usually don’t appear all at once. The most frequently observed manifestation is Raynaud’s phenomenon (RP), found in 75–90% of patients.
Epidemiology
MCTD is a rare disease, and the exact incidence is unknown. A population-based study from Olmsted County, Minnesota found that MCTD occurred in about 2 persons per 100,000 per year and in Norway found the point prevalence rate to be 3.8 cases per 100,000 adult population. MCTD is more common in females than in males. Estimates of the female-to-male ratio vary from approximately 3:1 to 16:1.
Risk factors and possible causes
The exact cause of MCTD is unknown, but there are several recognized risk factors that may contribute to the development of this disease:
- Genetic factors
- Environmental factors: exposure to certain viral infections or chemical substances may play a role in the development of MCTD
- Gender: MCTD is more commonly diagnosed in women; the disease is estimated to affect women about nine times more frequently than men
- Age: MCTD can occur at any age, but it most commonly affects individuals between the ages of 20 and 30
Common symptoms
Joints:
- Arthralgia (up to 86%) – joint pain mostly early in the morning / during the night
- Arthritis (joint inflammation – tender, warm, and swollen joints) (70%)
- Prolonged morning stiffness – painful and limited joint mobility
Muscles:
- Myalgia – pain in muscles
- Muscle weakness
Skin lesions:
- Raynaud’s phenomenon (up to 96%)
- Sclerodactyly – thickening and tightness of the skin of the fingers or toes
- Puffy hands – swelling of the hands with thickening of the fingers
- Livedo reticularis – a mottled reticulated vascular pattern that appears as a lace-like purplish discoloration of the skin
- Telangiectasia – small dilated blood vessels located near the surface of the skin or mucous membranes
- Various skin rashes – sun-sensitive rash (on sun-exposed areas, such as the face, neck, or anterior upper chest), malar rash on the face, lesions typically seen in DM (ie. Gottron signs, purple discoloration on the eyelids)
- Hair loss – local or general
Eyes:
- Dry eyes (30%) – decreased production of tears leading to itching, redness, pain, and the feeling of sand in the eyes
- Conjunctivitis
Autoimmune thyroid disease
Lungs:
- Pleuritis – inflammation of the pleura
- Interstitial lung disease – manifested as cough, shortness of breath, or flu-like symptoms
- Pulmonary arterial hypertension – caused by thickening and narrowing the lung arteries, that raises the blood pressure in the lungs and causes heart overload
Heart:
- Pericarditis – inflammation of the pericardium around the heart; is the most frequent manifestation of heart involvement, but nevertheless it is relatively rare
- Irregular heartbeat
Gastrointestinal:
- Gastrointestinal tract hypomotility, especially esophageal hypomotility – presents as difficulty with swallowing, chest pain and heartburn
- Oral ulcers – sores inside the mouth
- Dry mouth (30%) – decreased production of saliva
- Splenomegaly – enlarged spleen
- Hepatomegaly – enlarged liver
Hematological disorders:
- Anemia – low red blood cells count or low hemoglobin
- Leukopenia – low white blood cell count
- Thrombocytopenia – low platelet count (manifested as easy bruising, gum bleeding)
Neurological disorders:
- Peripheral neuropathy – abnormal nerve sensations in the face or limbs
Constitutional symptoms:
- Fever
- Fatigue – tiredness, lack of energy and motivation
- Weight loss
What is Raynaud’s phenomenon and how to manage it?
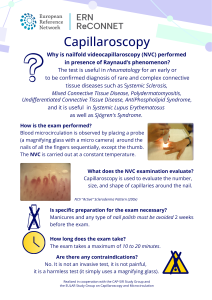
Raynaud’s phenomenon (RP) can be primary (on its own) or secondary (along with other diseases like SLE, SSc, or MCTD). RP results from prolonged vasoconstriction of the small vessels causing decreased blood flow to the fingers, rarely toes, usually provoked by cold, stress, or emotional upset. RP manifests as white-pale, blue, and red fingers with pins and needles sensations, discomfort, and pain. The symptoms resolve spontaneously. In severe cases of secondary RP, prolonged vasoconstriction can lead to digital ulceration or gangrene. The diagnosis is established based on the patient’s history and physical examination. Usually, the doctor performs nailfold capillaroscopy to examine the blood vessels below the fingernails.
General recommendations for RP
- Keep the body warm and avoid exposure to cold and sudden temperature changes. Try not to go quickly from heat to air conditioning
- Manage stress. Stress can trigger Raynaud’s symptoms
- Quit smoking, but also avoid passive smoking! Smoke causes skin temperature to drop
- Avoid hand injuries. In patients with RP, hand injuries can take longer to heal
- Exercise. Exercise increases blood flow
During an RP attack
- Immediately get indoors or to a warmer area
- Massage your hands and feet
- Wiggle your fingers and toes
- Place your hands under your armpits or un your warm belly
- Make wide circles with your arms
- Run warm (not hot!) water over your fingers and toes
When to see a doctor ?
You should seek medical attention if:
- You experience any of the aforementioned symptoms
- Your current symptoms worsen
- You notice any new signs and symptoms
- You are not tolerating the treatment prescribed by the doctor
How to prepare for the doctor’s visit
- Arrive early, as you may need to complete forms.
- Clarify what your main symptoms are. Think about your complaints and try to describe them as best you can. If you are a new patient, you can compile a diary/list with your complaints and other health problems.
- Bring all prior medical documents (tests, letters, X-rays, etc.).
- Bring a list of the medicines you take. Remember the side effects of relevant current or prior medications.
- Remember to tell your doctor other details about your health, such as vaccination schedules, allergies, and family health history.
- Bring a family member if you are nervous and afraid you could miss discussion points during your appointment.
- At the end of the consultation, make a note of your next appointment and ask how to proceed if you have an urgent health problem or cannot tolerate the medication.
Diagnosis
Diagnostic path
- Find the Medical Center – Click here (A map of ReCONNET centers)
- Medical interview with a doctor – Click here (How to prepare for a Doctor visit).
- The doctor may refer you for lab tests, other tests (ultrasound, X-rays, etc.), or other specialists.
- You will have a follow-up visit after collecting all the necessary test results and medical consultations.
- At the follow-up visit, the doctor may confirm a suspected diagnosis, refer for more tests or rule out a suspected diagnosis.
- Once the diagnosis is established, the doctor will discuss further treatment with you.
- Since the disease can evolve into a defined connective tissue disease, it is essential to visit your doctor regularly.
Diagnostic tests
Laboratory tests – usually the standard panel includes the following, but it vary depending on clinical presentation:
- Complete blood count (CBC)
- C-reactive protein (CRP), Erythrocyte sedimentation rate (ESR) – inflammatory markers
- Routine parameters to asses organ function (such as serum creatinine, liver function tests, muscle enzymes)
- Urinalysis with microscopic analysis
- Protein electrophoresis
- Antinuclear antibodies (ANA) and ANA profile
- Rheumatoid factor and anti-CCP
Imaging studies
- X-rays
- Ultrasounds
- Echocardiography
- CT scanning
- MRI
- Capillaroscopy – non-invasive technique to evaluate small vessels of the microcirculation in the nailfold
Other tests
- Pulmonary function tests (PFT) , the 6-minute walk test (6MWT) – to asses cardiopulmonary insufficiency
- Schirmer’s test – to assess whether the eye produces enough tears to keep it moist
- Electrocardiogram (ECG)
- Esophageal manometry
- Electromyography (EMG)
- Electroneurography (ENG)
Criteria of MCTD diagnosis
There are several different sets of diagnostic criteria for MCTD. The patient may be diagnosed with MCTD if he meets the following commonly used criteria:
- by Alarcon-Segovia D, Villareal M., which consist of the presence of anti-U1-RNP antibodies and at least three of the following clinical symptoms: 1. edema of the hands, 2. synovitis, 3. myositis, 4. Raynaud phenomenon, 5. sclerodactyly
- or the Kasukawa one, that divides the symptoms into groups and in every one of them at least one symptom must be present: i) common symptoms: 1. Raynaud phenomenon, 2. swollen fingers or hands; ii) positive anti-U1-RNP antibodies; iii) ‘Mixed’ symptoms such as: a) SLE-like ones: polyarthritis / lymphadenopathy / facial erythema / pericarditis or pleuritis / leukopenia or thrombocytopenia; b) SSc-like ones: sclerodactyly / lungs involvement / esophageal involvement; c) Polymyositis-like ones: muscle weakness / raised muscle enzymes / myogenic pattern of EMG
Differential diagnosis
Due to the significant heterogeneity of the disease presentations, in differential diagnosis should be considered neoplastic processes, infections, other connective tissue diseases (such as SLE, SSc, RA, inflammatory myopathies), idiopathic pulmonary arterial hypertension.
Treatment overview
Treatment in MCTD should be individually tailored to each patient, taking into account the specific organs affected by the disease and the severity of disease course. Main groups of medications used in MCTD are:
- Nonsteroidal anti-inflammatory drugs – to control musculoskeletal pain and inflammation
- Glucocorticoids (GCs) – used to induce remission in case of flare-up
- Immunosuppressant agents like methotrexate or azathioprine – to control severe symptoms
- Phosphodiesterase inhibitors, endothelin receptor antagonists, or prostaglandins – for pulmonary hypertension
- Antimalarial drugs (ex. hydroxychloroquine) – usually in case of skin rashes, photosensitivity, or articular symptoms
- Calcium channel blockers like amlodipine or nifedipine – in the case of Raynaud’s phenomenon
- Sunblock lotions
- Protective measures in case of exposure to cold
Additionally, for improving the quality of life, it is important to engage in appropriate physical activity, maintain a balanced diet, and reduce stress.
Prognosis
MCTD is a chronic disease and currently is not fully curable. However, a substantial part of the patients have a favorable outcome, sometimes achieving complete long-term remission. Internal organs involvement significantly worsens the prognosis. The mortality rate after 10-12 years varies between 8 and 36% and the most common cause is pulmonary hypertension, followed by infections and malignancies.
References
CLINICAL OVERVIEW
Chaigne B, et al. Mixed connective tissue disease: state of the art on clinical practice guidelines. RMD Open. 2018.
Sharp GC, et al. Mixed connective tissue disease – an apparently distinct rheumatic disease syndrome associated with a specific antibody to an extractable nuclear antigen (ENA). Am. J. Med., 1972
EPIDEMIOLOGY
Ungprasert P, et al. Epidemiology of Mixed Connective Tissue Disease, 1985-2014: A Population-Based Study. Arthritis Care Res (Hoboken). 2016.
Gunnarsson R, et al. The prevalence and incidence of mixed connective tissue disease: a national multicentre survey of Norwegian patients. Ann Rheum Dis. 2011.
Greidinger E.L. et al., Mixed Connective-Tissue Disease (MTCD). Medscape 2022.
COMMON SYMPTOMS
Greidinger E.L. et al., Mixed Connective-Tissue Disease (MTCD) Clinical presentation. Medscape 2022.
Gunnarsson R, et al. Mixed connective tissue disease. Best Pract Res Clin Rheumatol. 2016.
DIAGNOSIS AND PROGNOSIS
Alarcon-Segovia D, Villareal M. Classification and diagnostic criteria for mixed connective tissue disease. In: Mixed connective tissue diseases and antinuclear antibodies. Kasukawa R, Sharp GC (eds.). Elsevier; Amsterdam 1987; 33-40.
Kasukawa R, Tojo T, Miyawaki S. Preliminary diagnostic criteria for classification of mixed connective tissue disease. In: Mixed connective tissue diseases and antinuclear antibodies, Kasukawa R, Sharp GC (eds.). Elsevier; Amsterdam 1987; 41-47.
Sapkota B, Al Khalili Y. Mixed Connective Tissue Disease. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
Tani C, Carli L, et al. The diagnosis and classification of mixed connective tissue disease. J Autoimmun. 2014.
TREATMENT OF MIXED CONNECTIVE TISSUE DISEASE
Kim P, Grossman JM. Treatment of mixed connective tissue disease. Rheum Dis Clin North Am. 2005.
Greidinger E.L. et al. Mixed Connective-Tissue Disease (MCTD) Medication. Medscape. 2022.
THE STORY OF A PATIENT WITH MCTD: Living with MCTD: A phoenix attempt – Rare Disease Day 2023
ERN ReCONNET publications are available for consultation.
LIST OF USEFUL REFERENCES
1. 2019 Diagnostic criteria for mixed connective tissue disease (MCTD): From the Japan research committee of the ministry of health, labor, and welfare for systemic autoimmune diseases
Tanaka Y, Kuwana M, Fujii T, Kameda H, Muro Y, Fujio K, Itoh Y, Yasuoka H, Fukaya S, Ashihara K, Hirano D, Ohmura K, Tabuchi Y, Hasegawa H, Matsumiya R, Shirai Y, Ogura T, Tsuchida Y, Ogawa-Momohara M, Narazaki H, Inoue Y, Miyagawa I, Nakano K, Hirata S, Mori M.
Mod Rheumatol. 2021 Jan;31(1):29-33.
2. Recommendations for screening and detection of connective tissue disease-associated pulmonary arterial hypertension
Khanna D, Gladue H, Channick R, Chung L, Distler O, Furst DE, Hachulla E, Humbert M, Langleben D, Mathai SC, Saggar R, Visovatti S, Altorok N, Townsend W, FitzGerald J, McLaughlin VV; Scleroderma Foundation and Pulmonary Hypertension Association.
Arthritis Rheum. 2013 Dec;65(12):3194-201.
Tanaka Y, Kuwana M, Fujii T, Kameda H, Muro Y, Fujio K, Itoh Y, Yasuoka H, Fukaya S, Ashihara K, Hirano D, Ohmura K, Tabuchi Y, Hasegawa H, Matsumiya R, Shirai Y, Ogura T, Tsuchida Y, Ogawa-Momohara M, Narazaki H, Inoue Y, Miyagawa I, Nakano K, Hirata S, Mori M.
Mod Rheumatol. 2021 Jan;31(1):29-33.
Khanna D, Gladue H, Channick R, Chung L, Distler O, Furst DE, Hachulla E, Humbert M, Langleben D, Mathai SC, Saggar R, Visovatti S, Altorok N, Townsend W, FitzGerald J, McLaughlin VV; Scleroderma Foundation and Pulmonary Hypertension Association.
Arthritis Rheum. 2013 Dec;65(12):3194-201.
2. Sharp GC et al., Diagnosis criteria for classification of MCTD. In Kasukawa R, Sharp GC., Mixed connective tissue disease and antinuclear antibodies. Amsterdam, Elsevier Science. 1987. 151-178.
3. Alarcon-Segovia D et al., Classification and diagnosis criteria for mixed connective tissue disease. In Kasukawa R, Sharp GC. Mixed connective tissue disease and antinuclear antibodies. Amsterdam, Elsevier Science. 1987. 33-40.
4. Kasukawa R et al., Mixed connective tissue disease and antinuclear antibodies. Amsterdam, Elsevier Science. 1987. 357.
MCTD centres in ERN ReCONNET
Helsinki University Hospital, Hospital District of Helsinki and Uusimaa, Finland (ReCONNETFIN) (adult and paedriatric)
- AOU Careggi, Florence
- AOU Meyer di Firenze (paediatric)
- Foundation IRCCS CA’Granda Ospedale Maggiore polyclinic – Milan
- ASST Centro Specialistico Ortopedico Traumatologico Gaetano Pini (Presidio Pini)
- AO Padua
- AOU Pisan
- AOU Policlinico Umberto I di Roma
- Fondazione Policlinico Tor Vergata Roma
- AOU S. Giovanni di Dio e Ruggi D’Aragona
- A.S.L. Torino – Hub S. Giovanni Bosco
- Azienda Ospedaliera Universitaria Integrata di Verona
University Medical Centre Ljubljana (paediatric)
Hospital Clínic de Barcelona y Hospital de Sant Joan de Déu (adult and paediatric)